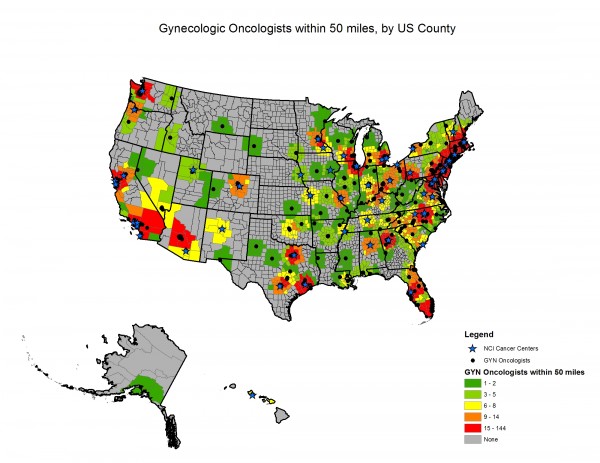
According to a recent study published in the journal Gynecologic Oncology, conducted by researchers from the Perelman School of Medicine at the University of Pennsylvania, about one-third of US counties are located at a distance of 50 miles or more from the nearest gynecologic oncologist, impacting access to gynecologic care complexes for about 15 million women with ovarian and other gynecologic cancers. Moreover, most counties with limited access are located in the Midwest and Mountain-West regions, while counties with more specialists are located on the Atlantic coast between the Atlanta and Boston areas.
“This is the first national study to identify specific regions of the United States where residents may be at an increased risk for poor clinical outcomes – including misdiagnoses and late detection – as a result of limited access to specialized gynecologic cancer care,” said David Shalowitz, MD, a fellow in the division of Gynecologic Oncology at the Perelman School of Medicine at the University of Pennsylvania, and lead study author. “Based on our estimates, it’s likely that more than 7,000 women with gynecologic cancers per year experience distance–related barriers to accessing appropriate care from a specialist. Increased travel time to a specialty center likely prevents many patients from being appropriately evaluated, and may decrease their likelihood of receiving the standard of care, or accessing clinical trials for ovarian, uterine and cervical cancers,” he added.
To assess the amount of gynecologic oncologists situated within 50, 100 and 150 miles of county borders, researchers used spatial analysis including more than 3,000 US counties. The results revealed that about 36% of the counties were situated more than 50 miles from the nearest specialist, resulting in limited access to about 14.8 million women.
With the exception of Wyoming and North Dakota, all states had a minimum of one gynecologic oncologist. The results also showed that all of North Dakota is situated more than 50 miles from the closest specialist.
The team also found that 15% of women experience care barriers caused by their referral network, and that a total of 123 national referral networks do not have specialist access, indicating that, in order to have contact with a gynecologic oncologist, women need to travel outside of their referral network.
“Nine to 15 percent of women live in areas that likely limit their access to high-quality care for these potentially deadly conditions,” said Dr. Shalowitz in the news release. “While we don’t yet know how access correlates to health outcomes, referral networks need to be structured in a way that alleviates the burden of travel for women in need of a specialist.”
The authors believe other studies should determine the areas with poorer clinical outcomes as a consequence of geographic locations and there should be an effort to produce a geographically-linked comprehensive national database concerning gynecologic cancer care and patients’ clinical outcomes.