Patients with persistent or recurrent metastatic carcinoma of the cervix (PRmCC) may strongly benefit from treatment with Advaxis‘ experimental vaccine axalimogene filolisbac (AXAL), according to preliminary data from the second stage of a Phase 2 clinical trial.
The single-arm, open-label Phase 2 GOG-0265 trial (NCT01266460) showed acceptable tolerability and promising activity, with AXAL treatment inducing a 50 percent increase in patients’ expected 12-month overall survival. The study was conducted by the Gynecologic Oncology Group (GOG), which is now part of NRG Oncology.
“These data demonstrate a meaningful improvement in 12-month overall survival rate compared to historical GOG studies,” Warner K. Huh, MD, division director of gynecologic oncology at the University of Alabama at Birmingham and lead investigator of the study, said in a press release.
“Historical survival rates for patients with PRmCC underscore the need for additional treatment options for patients and these results illustrate the promising therapeutic potential for axalimogene filolisbac in women with this rare cancer,” Huh said.
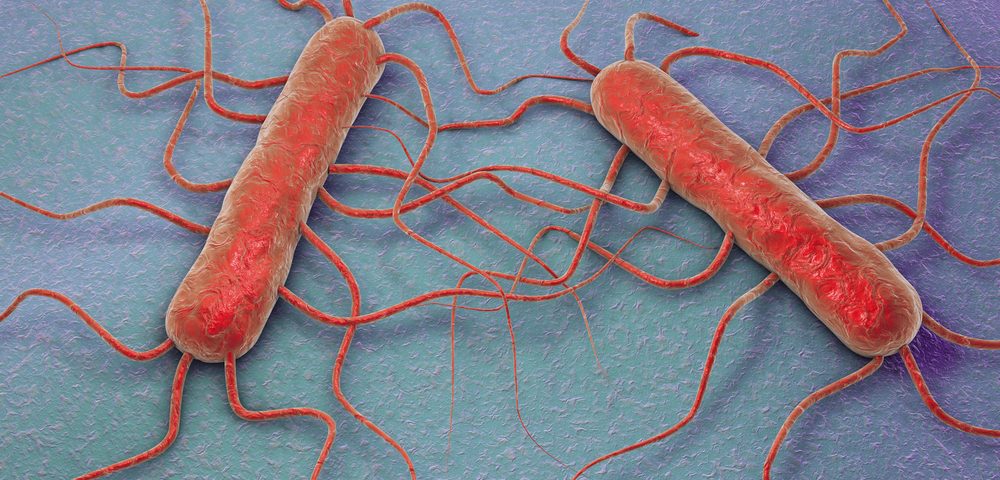
Axal is a new vaccine approach that uses the live attenuated bacteria Listeria monocytogenes genetically altered to present the HPV-16 protein at the surface. The protein is then recognized by T-cells, which will become specific to HPV-positive cancer cells.
The study was supported by the Cancer Therapy Evaluation Program (CTEP) of the National Cancer Institute (NCI). It was designed to evaluate the activity and safety of Axal in PRmCC patients who had progressed on at least one prior systemic therapy in two stages.
The first stage included 26 patients who received intravenous AXAL on the first day of 28-day cycles until disease progression or unacceptable toxicity. The study met the the predetermined safety and effectiveness criteria required to proceed to the second stage, with AXAL treatment resulting in a 38.5 percent 12-month overall survival rate.
The second stage, which was amended to allow increased dosing, included 24 patients treated with Avastin (bevacozumab) and has now shown a 12-month overall survival of 37.5 percent. But due to a clinical hold that affected Advaxis’ clinical development programs, the second stage was not completed as designed.
According to Advaxis, the clinical hold was placed in October 2015 following the death of one patient who took AXAL in 2013 and cultured positive for Listeria monocytogenes,
But following an investigation, Advaxis concluded that the positive culture for the bacteria was likely related to the medical implants the patient received after having a car accident between her first and second AXAL doses. the investigator also concluded the death was due to cervical cancer progression and that AXAL played no role in the patient’s death, leading the U.S. Food and Drug Administration (FDA) to lift the clinical hold in December 2015.
Despite the hold, 12-month overall survival was consistent with that observed in the first stage of this clinical trial. And based on the prognostic factors of the patients enrolled in both stages of the study, the researchers expected a 25 percent 12-month overall survival, suggesting that AXAL treatment increased the one-year overall survival by 52 percent.
In the second stage of the study, 62.5 percent of patients experienced a grade 1 or grade 2 treatment-related adverse event, with the most common being hypotension, nausea, chills, and fever. Grade 3 adverse events were observed in 37.5 percent of patients, and 8 percent experienced grade 4 adverse events.
“We are very encouraged by these data and look forward to presenting and discussing a more detailed analysis of the trial results at an upcoming medical society meeting,” said Daniel J. O’Connor, president and CEO of Advaxis. “We believe that a more than 50 percent increase in 12-month overall survival rate is clinically meaningful, and Advaxis plans to pursue registrational opportunities in Europe in 2017.”
AXAL has already been granted fast track designation by the FDA to treat high-risk locally advanced cervical cancer following surgery to remove the tumor, and was granted orphan drug status to treat invasive cervical cancer.