Different gene variants, also referred to as single nucleotide polymorphisms (SNPs), can affect susceptibility to cancer. A recent study has uncovered the molecular mechanism underlying why patients with a specific SNP in the NKG2D gene are less likely to develop human papillomavirus (HPV)-associated cancers, including cervical cancer.
The study, “A functional polymorphism in the NKG2D gene modulates NK-cell cytotoxicity and is associated with susceptibility to Human Papilloma Virus-related cancers,” was published in Scientific Reports.
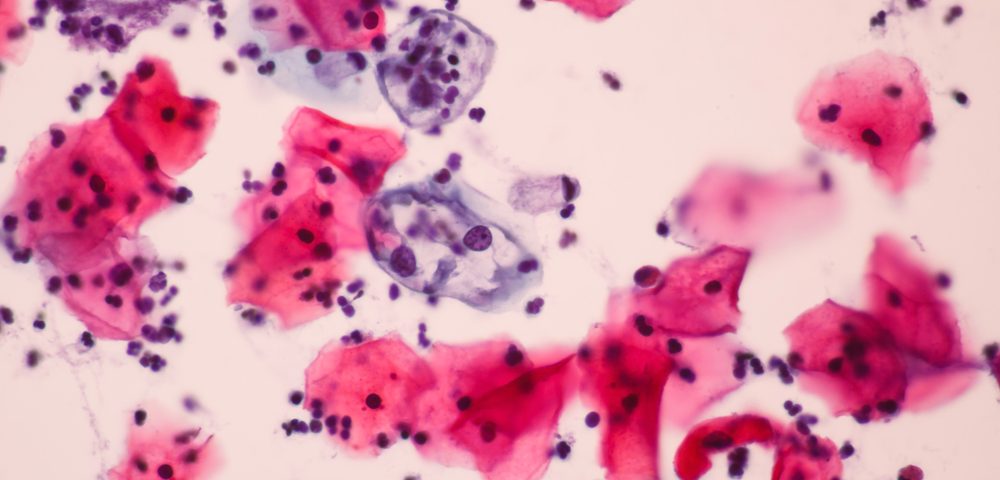
Immunosurveillance ensures that cancer cells are eliminated by the innate immune system before they are allowed to replicate. Natural killer (NK) cells are the primary effector of this system and, when activated, initiate cell death of both infected cells and tumors. NKG2D encodes for a transmembrane protein that functions as an activating receptor on NK cells. Previous reports have shown that the NKG2D gene variant, referred to as rs1049174, can affect cancer susceptibility.
Indeed, while NK cells expressing the normal NKG2D variant show high cytotoxicity, which is the ability to kill tumor cells, those with the rs1049174 gene variant have low cytotoxicity. Therefore, previous studies have shown that people with the high cytotoxicity genotype (HNK/HNK) are less susceptible for developing cancers, while those with the low cytotoxicity genotype (LNK/LNK) are more susceptible.
Now, researchers have shed some light on the mechanisms mediating this effect, exploring the functional implications of the NKG2D gene variants.
Looking into DNA samples from 153 Vietnamese women with cervical cancer and 123 Vietnamese patients with genital cancers (anal, penile,vulvar, or vaginal), the authors confirmed the role of the NKG2D gene variants in cancer susceptibility. They found that controls had a low incidence of the LNK/LNK variant, compared to those who developed cancers. Similarly, patients with genital cancer and HPV-associated cancer were less likely to exhibit the HNK/HNK variant compared to controls.
The researchers explored the functional significance of this specific NKG2D variant to better understand why it affected cancer susceptibility. They found that patients with the low-susceptibility variant (HNK/HNK) had higher levels of NKG2D in NK cells compared to those with the LNK/LNK variant.
More in-depth analysis showed that the presence of the HNK variant enhanced expression of NKG2D by preventing the binding of a specific microRNA inhibitor — miR-1245. MicroRNAs are small RNA molecules that impair the production of a functional protein.
Because NKG2D functions as an activator of NK cells, the higher expression of NKG2D in patients with the HNK/HNK genotype suggests that the activity of natural killer cells is enhanced.
Indeed, the authors find that the NGK2D variant affects NK cell activity. When the HNK/HNK variant is expressed in NK cells, these cells have increased ability to kill tumor cells, particularly HPV+ cells, when compared to cells expressing the LNK/LNK genotype. This provides a molecular mechanism describing that patients with the LNK/LNK genotype are more susceptible to HPV+ cancers due to their lowered immunosurveillance and decreased ability to destroy tumour cells.
Presence of the HNK/HNK variant, conversely, causes higher expression of NKG2D and higher activity of NK cells, leading to increased elimination of tumor cells. When tumor cells can be efficiently destroyed, cancer susceptibility is lessened.
This study proposes a model for the superiority of the HNK/HNK genotype among the NKG2D gene variants. It adds to the broader body of evidence regarding the role of NKG2D in cancer risk.