Women with moderate-to-severe changes in their cervical cells who don’t get follow-up testing or treatment are four times more likely to develop cervical cancer than women who receive treatment, according to researchers from the Ontario Cervical Screening Program and Cancer Care Ontario.
The study, “Are Women Who Exit Colposcopy Without Treatment at Elevated Risk for Cervical Cancer?,” published in the Journal of Lower Genital Tract Diseases, highlights the need for centralized programs ensuring that women with cervical abnormalities are not discharged prematurely and receive subsequent screening.
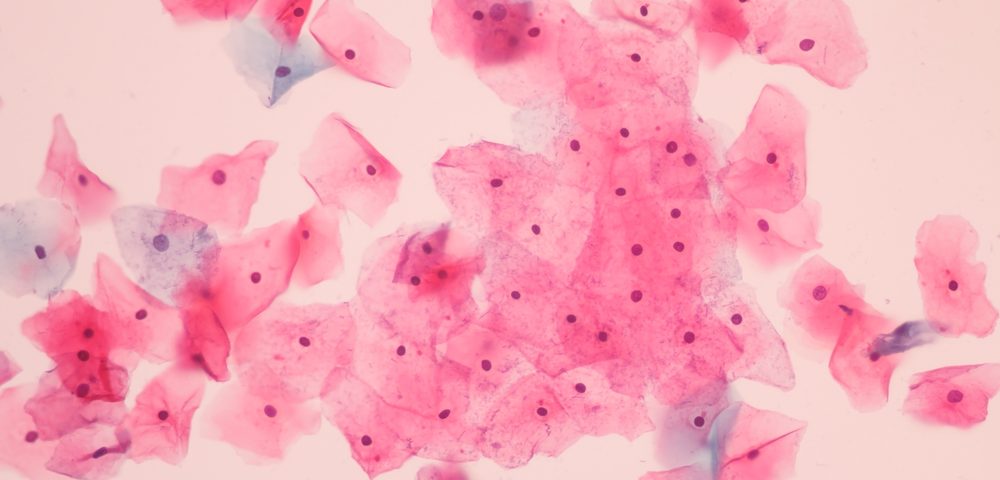
Cancer Care Ontario, the Ontario government’s advisor on cancer and access to key health services, recommends women aged 21 to 69 years who are sexually active get a Pap test every three years. This test checks for abnormal cervical cancer cells that could evolve into cervical cancer.
If the Pap test results come back abnormal, women may need a follow-up procedure, called colposcopy, where a doctor closely examine the cervix, vagina, and vulva, looking for signs of disease. If an unusual area of cells is found during colposcopy, doctors may take a tissue sample for analysis. In some cases, women may need more than one colposcopy to remove the abnormal-looking tissues.
To estimate the impact of treatment and follow-up colposcopy in the risk of cervical cancer, doctors examined data from 14,787 women with mild cervical abnormalities, and 41,916 women with moderate-to-severe abnormalities, detected for the first time between 2007 and 2010, who underwent colposcopy within one year.
By March 2015, 28.5% and 62% of women with mild or severe abnormalities, respectively, received treatment. But nearly a third of women received only one colposcopy (37% and 28%, respectively).
The researchers found that women with severe abnormalities who did not receive treatment had increased incidence of cervical cancer, compared to those who were treated (1.1% vs. 0.3%).
Results also showed that women with severe abnormalities who received only one colposcopy and no treatment were 6.6 times more likely to develop cervical cancer than those who received treatment and multiple colposcopies.
For women with mild abnormalities, treatment and no-treatment groups had similar incidence rates (.08% in both groups), but those who received only one colposcopy were nearly four times more likely to develop cervical cancer than those with multiple colposcopies, irrespective of treatment.
“While some lesions detected during colposcopy do not require immediate treatment, these findings demonstrate the importance of ensuring that women are receiving appropriate and timely follow-up care,” Rachel Kupets, MD, said in a press release. Kupets is scientific lead for the Ontario Cervical Screening Program (OCSP) with Cancer Care Ontario, and co-author of the study.
The authors also found that the risk of women with moderate to severe cervical abnormalities who did not receive follow-up testing or treatment saw their risk of cervical cancer increase with age. Women in the 60-to 69-year-old cohort were found to have the highest risk.
“Developing a clear set of guidelines for colposcopists, physicians and nurses would help ensure that all women are being properly monitored and no lesions are missed,” Kupets said.